Frequently asked questions (FAQ) on acute drug toxicity presentations to hospital emergency services
What is acute drug toxicity?
Acute drug toxicity is defined as the unwanted effect(s) (such as anxiety, hallucination, coma…) that may occur either immediately or at a short time interval after the uptake of one or more drugs (more details about the inclusion and exclusion criteria used in our monitoring are available below).
Why does acute drug toxicity matter?
Worldwide, high-risk drug use results in a considerable burden of mortality and morbidity. One important cause of morbidity among both high-risk drug users and more occasional, recreational drug users, relates to acute drug toxicity (i.e. toxicity which arises soon after use). There are an estimated 1.2 million non-fatal overdoses per year worldwide amongst injecting drug users (1). Every year in Europe, thousands of people present to hospital emergency services with an acute drug toxicity related to the use of illicit drugs, sometimes with prescription medicines and/or alcohol. To monitor this phenomenon, and to support evidence-based policies to respond to drug-related harm, the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) collects and analyses data on acute drug toxicity presentations to sentinel hospitals across Europe through the European Drug Emergencies Network (Euro-DEN Plus).
What does it tell us about drug use and drug-related harms?
Data from hospital emergency services are a direct indicator of acute health harm due to drug toxicity and an indicator of trends in both high-risk drug use and recreational drug use. This data is also a source of information to characterise the acute toxicity presentations by age, gender, time, place and severity. Additionally, the monitoring of the acute drug toxicity presentations can signal new patterns of use, increasing/decreasing use of some drugs (such as crack, nitrous oxide, new synthetic drugs), or new trends regarding traditional drugs such as MDMA, or prescription medicines such as opioids and benzodiazepines in the context of polydrug use.
How does the EMCDDA monitor acute drug-toxicity presentations to sentinel hospitals?
The EMCDDA has been supporting the European Drug Emergencies Network (Euro-DEN Plus) for several years. This project, which was EU-funded from 2013-15 and is now supported by the EMCDDA, involves the collection of data on emergency department presentations with acute drug toxicity from 32 sentinel centres in 22 countries. The network relies on volunteer emergency physicians and clinical toxicologists and researchers and monitors acute drug toxicity presentations to sentinel hospitals across Europe. While the presentations seen in the sentinel hospitals may not reflect the national picture and this is not a representative data set, it does provide insights on patterns and trends in drug-related emergency presentations. More centres are currently being recruited – with the aim to cover more countries and different types of locations – in order to inform local and global policy making and responses to the drug situation.
Information on related news, events and topics, and links to recent publications are available on the EMCDDA Hospital emergencies resource pages
What is the value of monitoring acute drug-toxicity presentations?
The Euro-DEN Plus network aims to provide information on the nature and extent of harms associated with the use of illicit drugs and misuse of prescription medicines. This project complements other information and indicators on drug consumption and potential emerging health threats and has the following adding value:
- widens the scope of monitoring health consequences of drug use, beyond routine indicators such as drug-related deaths and treatment demand.
- helps, along other indicators, to assess the burden of harms and to describe the toxicity of substances that less frequently cause fatal overdoses (such as cannabis and, to a lesser extent, stimulants), or do not necessarily lead to treatment requests for drug dependence (such as nitrous oxide, etc.)
- produces local and timely information that can be used for city-level monitoring and interventions. This is important because regional specificities exist both in term of drug use (e.g. recreational drug use in the night life economy) and responses available (e.g. referral procedures after discharge from hospital),
- contributes to understand better the risk factors for some severe outcomes, including e.g. psychosis, seizures, or admission to intensive care units (see more information in the list of peer reviewed publications)
- monitors polydrug use and in particular the possible impact of medicines and alcohol (see more information in the list of peer reviewed publications)
- contributes to early warning systems on new synthetic drugs, as the sentinel emergency services might capture signals earlier and with more sensitivity than monitoring systems based on hospital routine data
- complements the national data reported from the Focal Points to the EMCDDA in this area, noting that national data on acute drug-related harm usually underestimates the extent of the problem and may provide a biased picture (2-4).
What are the ethical and data protection considerations in place?
Each Euro-DEN Plus sentinel centre has appropriate local ethical approval in place to be able to collect and share the Euro-DEN Plus dataset. Data are pseudonymised and no individual data is identifiable in any published material from the project. The project only collects data recorded as part of the routine management of the cases (i.e. there is no additional clinical examination, investigation or intervention carried out).
Are there differences across participating hospitals?
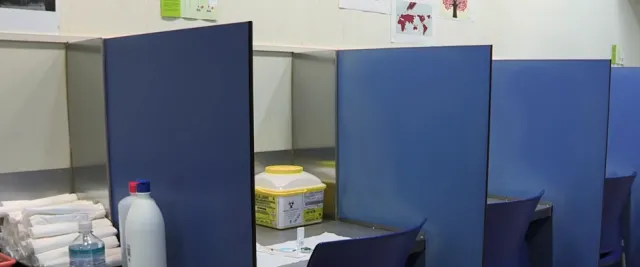
The network is constituted by a variety of hospitals, which differ in the estimated size of the population served, the number of beds, the drug using population they serve. The information is presented in the interactive map below.
What are the inclusion criteria?
All presentations with clinical features consistent with acute drug toxicity and/or directly related to acute drug use are included. Drug use may occur in the context of dependence, substance use disorders; for work purposes (performance); for recreational use, i.e. with occasional or regular use in recreational settings or occasions, without dependence (or substance use disorders).
Presentations are included if the drug(s) involved in the presentations are established illicit drugs, new psychoactive substances, plants, fungi or herbal/alternative medicines; licensed pharmaceutical preparations (both prescription and over the counter medicines) misused for recreational purposes or in the context of substance use disorder; or industrial and/or domestic products (i.e. solvents, glues, propellants etc.) used for recreational purposes or in the context of substance use disorder.
The information on the drugs involved in the presentation can be derived from a combination of the following: the patient’s self-reported use; information retrieved from witnesses; the observation of the clinicians assessing the patient; and the toxicologist reviewing data entry/case records. If toxicological testing is undertaken as part of routine clinical care data on the results of this analysis is collected.
What are the exclusion criteria?
- Lone alcohol ingestion or intoxication, including cases involving ‘spiked drinks’ (i.e. drinks to which it is alleged a substance has been maliciously added) where patients have no clinical features of acute recreational drug toxicity
- Injury related to trauma, unless the trauma is directly related to drug use e.g. as a result of hallucinations
- Drug or ethanol (i.e. alcohol) withdrawal
- Secondary complications of chronic drug use (e.g. infected injection sites, HIV, HBV, HCV infections, endocarditis) or of previous acute drug use complications (e.g. previous stroke secondary to hypertensive intracranial haemorrhage presenting with aspiration pneumonia)
- If a patient attends the emergency room requiring treatment because s/he has been physically assaulted but it subsequently found that s/he has used drugs, the patient will not be included as the presenting complaint was not related to the drug use.
What data are collected?
Data are collected on the patient demographics (age, sex), the agent(s) used, the presentation observations, the clinical features (using a pre-defined list), the treatment given and the patient outcome. Analytical confirmation of the agents used is not routinely undertaken in all the centres. However, if analysis is undertaken as part of routine clinical care and the results are available this data is collected. Each centre also reports the total monthly number of attendances (for any reason) to the emergency room.
Is there laboratory confirmation of the drugs involved?
If drug screening is undertaken as part of routine clinical care, the results of this screening are collected, but drug screening is not undertaken specifically for the project. This follows international best practice in the management of acute drug toxicity, whereby patients are treated on the basis of the clinical pattern of toxicity and the drug(s) that the patient reports having used, rather than on the basis of routine analytical confirmation of the drugs involved.
Are there any caveats to take into account when intrerpreting this data?
The Euro-DEN Plus data reflect local patterns of drug use and drug-related harm, providing a powerful and valuable triangulation tool at city level. One limitation of this approach is that findings cannot be extrapolated to other cities or to the country in question as a whole. However, the expansion of the network to include multiple centres in some countries has helped to reduce this limitation.
What are the strengths of the sentinel approach?
The Euro-DEN Plus model provides more timely data compared to other sources such as mortality or treatment registers, and thus this approach supports rapid risk assessments. Besides, emergency rooms are ‘trend spotter’ settings, where ‘novelties’ in drug use, and harms caused by the most risky patterns of drug use are observed (e.g. injecting or mixing drugs). Furthermore, Euro-DEN Plus provides local level information for local policy making (e.g. hospitals near busy night life settings will see presentations related to recreational drugs, and they can alert the local communities and health and law enforcement authorities). More presentations in one specific area suggests that this area presents specific social risk factors and interventions may be required. Finally, the sentinel approach allows triangulation with other local, regional or national datasets which proved valuable and insightful during recent the Trendspotter studies (5).
Are there some limitations?
There are several important limitations to keep consider when interpreting this data:
- There might be various ways to record and retrieve the data across hospitals as the source depends on local practices. However, the use of a common protocol limits the centre effect.
- A hospital within a city is not necessarily representative of the city as a whole, of the region or the country; local factors such as proximity to high concentrations of night-time economy venues, or social deprivation may impact on the types of presentations seen in the sentinel centre.
- The emergency services participating are mostly based in hospitals for adults; therefore, they rarely or do not see paediatric cases of acute drug toxicity. Other surveillance would be necessary to monitor the real burden and trends in acute drug toxicity among children and adolescents.
- Data is mostly self-reported and based on the clinician’s report (rather than toxicologically confirmed).
- For most cases, more than one drug is reported thus the effect of a particular drug in this context is difficult to assess.
- The dataset includes presentations and not patients. It likely includes repeat admissions on the same patient and therefore the observations may not be all independent. No information is collected to flag and count whether a person has presented in the past. If there are factors that predispose patients to present repeatedly, such patients will be over-represented in the sample of presentations.
- Numbers of cases are small in some hospitals. Therefore, the interpretation of percentages, the interpretation of changes and the comparisons overtime and across centres should be made cautiously.
- Some few centres collect a large part of the overall data and this should be kept in mind when interpreting the overall data. Local analysis is more informative than the global analysis.
- This monitoring is based on hospital emergency services and provides information only on the presentations to these settings. Other acute drug toxicity episodes do not result in presentations to hospitals and are therefore not captured. Presenting to emergency services might depend on the severity of the adverse effects, but also on the organisation of pre hospital care and referrals to hospitals in the country.
References
1. Colledge S, Peacock A, Leung J, Larney S, Grebely J, Hickman M, et al. The prevalence of non-fatal overdose among people who inject drugs: A multi-stage systematic review and meta-analysis. Int J Drug Policy. 2019;73:172-84.
2. Heyerdahl F, Hovda KE, Giraudon I, Yates C, Dines AM, Sedefov R, et al. Current European data collection on emergency department presentations with acute recreational drug toxicity: gaps and national variations. Clin Toxicol (Phila). 2014;52(10):1005-12.
3. Wood DM, Conran P, Dargan PI. ICD-10 coding: poor identification of recreational drug presentations to a large emergency department. Emerg Med J. 2011;28(5):387-9.
4. Wood DM, De La Rue L, Hosin AA, Jurgens G, Liakoni E, Heyerdahl F, et al. Poor Identification of Emergency Department Acute Recreational Drug Toxicity Presentations Using Routine Hospital Coding Systems: the Experience in Denmark, Switzerland and the UK. J Med Toxicol. 2019;15(2):112-20.
5. EMCDDA. Impact of COVID-19 on drug markets, use, harms and drug services in the community and prisons. Luxembourg: Publications Office of the European Union; 2021 April 2021. Report No.: 978-92-9497-580-5.
Other resources
Peer reviewed publications from the Euro-DEN Plus network: https://pubmed.ncbi.nlm.nih.gov/?term=euro-den&sort=date
The Euro-DEN network has also contributed to the European Drug Report since 2015